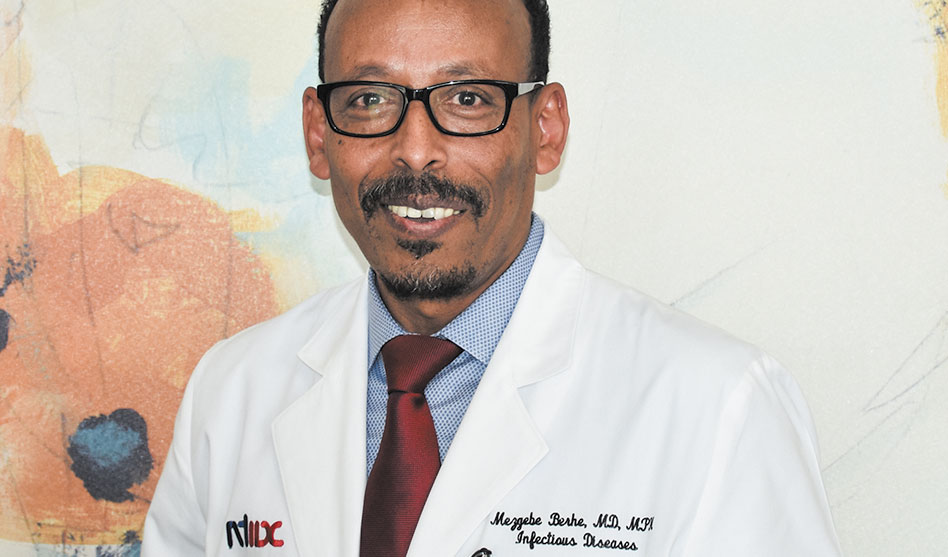
Dr. Mezgebe Berhe
Some HIV patients now eligible for study at NTIDC
Tammye Nash | Managing Editor
nash@dallasvoice.com
Pfizer Inc. announced over the weekend that the company has expanded enrollment in the company’s ongoing Phase 3 clinical trial of a vaccine for COVID-19 to up to about 40,000 participants, an expansion that allows for “the enrollment of new populations.”
For the researchers conducting the Pfizer Phase 3 trials at North Texas Infectious Disease Consultants, that means there is now room in the vaccine trial for certain of the practice’s HIV-positive patients, according to NTIDC’s Dr. Mezgebe Berhe.
“Enrollment in the trial has been proceeding as planned,” according to a press release dated Sept. 12, and the company “expects to reach its initial target of up to 30,000 participants [this] week. The proposed expansion would allow the companies to further increase trial population diversity and include adolescents as young as 16 years of age and people with chronic, stable HIV, Hepatitis C or Hepatitis B infection, as well as provide additional safety and efficacy.”
Dr. Berhe said NTIDC researchers have been “pushing for this” expansion in enrollment specifically to have the chance to include some of their HIV patients, as well as some of those with Hep C and Hep B. “We want our stable HIV patients to be able to participate because we want them to have that 50 percent chance” at getting the protection against COVID that the vaccine will hopefully provide.
The “50 percent chance” he referred to comes from the fact that half of the participants in the clinical trial will receive the vaccine, and the other half will receive a placebo. Berhe explained that this is a “double-blind study,” which means that the researchers themselves don’t know which patients are getting the vaccine and which are getting the placebo.
Berhe said to be considered for the vaccine, those with HIV must be on medication, under a doctor’s care and have their HIV under control.
“We are vaccinating about 20 people a day, five days a week right now,” he said. “We are hoping to give as many people as possible the opportunity to get this vaccination.”
Don’t rush the science
Berhe said there are currently more than 25,000 people nationwide enrolled in the Pfizer vaccine study. “Right now,” he continued, “we [at NTIDC] have vaccinated more than 300 people.” With the newly expanded enrollment protocols, that number will grow. He said that Phase 1 trials are designed to include a small number of participants to determine the safety of possible vaccines; Phase 2 trials include more participants and, while still testing for safety, are also intended to determine the effective dose at which the vaccine prompts an immune response.
Phase 3 trials include even more participants, and are designed to determine whether the vaccine is actually effective against, in this instance, COVID-19. “You give half the people a placebo and half the vaccine, then follow them over time, assuming similar exposure to COVID-19, to see the difference in how many go on to develop COVID-19,” the doctor said. “We want to see if the vaccine is effective in preventing infection, and if it is effective in keeping those who get infected from developing symptoms.”
He stressed that while no one expects to see a vaccine to be 100 percent effective, “what you want to see is a significant difference” in infections between those who receive the vaccine and those who receive a placebo.
In the U.S. right now, there are about 170 possible COVID-19 vaccines at various stages of development. “There are seven in Phase 3 trials, and 3 in Phase 2 trials,” Berhe said. “But the situation is very dynamic, so these numbers might not be totally accurate now.”
The process of developing a vaccine has, historically, taken about 10 years, from initial concept to distribution. One of the fastest vaccines in terms of the complete process was the mumps vaccine, introduced in 1967 after less than 5 years, Berhe said.
These days, he continued, in developing vaccines, “We have better medical technology, better platforms, just as in all areas of life” including things like computers and cell phones. “Because we have better technology, it is easier and faster to move through that process — from Phase 1, to Phase 2, to Phase 3, to approval,” Berhe said. “But even though we can get through this process faster now, the process itself should never be compromised, no matter what anybody says or wants.”
Because of the nature of COVID-19 — how easily it can spread and how deadly it can be — Berhe said the government has, thankfully, stepped up to provide the resources and funding to get an effective vaccine ready as soon as possible and then to distribute that vaccine as soon as it is ready.
But does that mean that the Trump administration’s efforts to rush a vaccine to distribution before the Nov. 3 election for political purposes are reasonable or possible?
“The government wants a vaccine as soon as possible,” Berhe said. “But there really is no way to predict when a vaccine is ready. And saying it will be ready before the election is probably the wrong concept.”
Berhe said he believes there will be a vaccine ready for distribution by the end of this year or the beginning of next year that will be effective at least in preventing the worst symptoms of the disease and hopefully effective in preventing infection and transmission. But one thing he knows for sure, without an effective vaccine, unlike other viruses such as Zika, “COVID-19 transmission is unlikely to end.”
Persons interested in participating in the vaccine trial should email vaccine.study@ntidc.org.